Full Text Article Open
Access 
Case
report
Non-bacterial
osteitis: Chronic Recurrent Multifocal Osteomyelitis
or pediatric SAPHO?
Triki
Ramy1,2,*,Daoudi Samih1,2,Guermazi
Bassem1,2,Kamoun Khaled1,2,Jlalia Zied1,2**,Jenzri Mourad1,2.
|
1: Department
of Pediatric Orthopedics Kassab
Institute, Ksar Said 2: College
of Medicine University
of Tunis El Manar Tunis
Tunisia * Corresponding
author ** Academic
Editor Correspondence
to: Trikiramy0816@gmail.com Publication
Data: Submitted:
March 5,2020 Accepted:
May19,2020 Online:
June 30,2020 This article was subject to full peer-review. This is
an open access article distributed under
the terms of the Creative Commons Attribution
Non-Commercial License 4.0 (CCBY-NC)
allowing sharing and adapting. Share:
copy and redistribute the material in any medium
or format. Adapt:
remix, transform, and build upon the
licensed material. the work
provided must be properly cited and cannot be used for commercial purpose. |
Abstract |
|
Chronic
Recurrent Multifocal Osteomyelitis (CRMO) and SAPHO syndrome represent the
group of autoinflammatory bone disease responsible
for recurrent non-bacterial osteitis (NBO). both are considered as defects of innate immunity. The
most common clinical presentation is recurrent episodes of bone pain with or
without fever.The clinical and imaging features are
non-specific.This usually leads to late and
confusing diagnosis. We
hereby report a case of CRMO in a 12-year-old patient. The aim is to
highlight the confusing overlap of clinical features between CRMO and SAPHO
syndromes. Keywords: multifocal osteomyelitis,
non-bacterial osteitis, SAPHO, bone pain. |
|
|
Observation A
12-year-old female patient with a history of recurrent metatarsalgia in the past year
presented with right thigh pain of three weeks duration. The pain was related
to exertion in the beginning and became permanent later. A fever of three
days duration preceded the onset of the pain. The examination revealed a
small painful swelling in the right thigh. Joint and skin examinations were
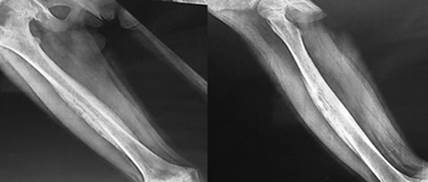
normal. X-rays
of right femur showed multilamellar inflammatory
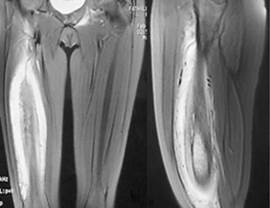
reaction of the shaft (Figure1). Magnetic resonance imaging (MRI) showed
heterogeneous mass withT1 hyposignal and T2 hypersignal which was diffusely infiltrating the muscles
(Figure 2). The
abdominal ultrasound and chest CT scan were normal. Laboratory exams revealed
high CRP and ESR. The hemoglobin rate was normal. The X-rays of both feet
showed multilamellar reaction of the 2nd
and 4th left metatarsal, bones and also of the right 2nd
metatarsal bone(Figure 3). MRI of the whole body
showed multiple lesions in the proximal and distal metaphysis of the left humerus, right humeral shaft, left acetabulum, pubic
rami, the right side of the sacrum and the right femoral neck (Figure 4).
Bone biopsies were performed from the femoral mass to rule out Ewing’s
sarcoma. Histopathology
examination showed non-specific chronic inflammatory cell reaction and
fibrosis. There was no sign of malignancy and the culture was sterile. Majeed syndrome was considered as differential but not
retained due to the absence of anemia and similar familial history. The
patient was treated by non-steroidal anti-inflammatory drugs and showed good
response. At 2-months follow-up there were satisfactory biological and
radiological improvements. |
|
Figure1 |
|
|
Figure 2 |
Figure 3 |
|
Figure 4 |
Figure
1: X-ray of the femur showing multilamellar
reaction Figure
2: MRI aspect of infiltrating right thigh mass Figure
3: X-rays of both feet
showing multiple metatarsal inflammatory processes. Figure
4: cartography of the different CRMO sites. |
Discussion
Typically,
CRMO presents as recurrent bone pain with or without low grade fever [1]. Episodic
exacerbations and remissions are characteristic. The bone pain has usually
insidious onset. Objective signs of arthritis may involve one or more joints
[2]. The skin findings include psoriasis, palmoplantar
pustulosis, pyoderma gangrenosum, and cystic scarring acne. The average age of
onset is 10 years (4-55years). Bone involvement in CRMO has usually an
asymmetric distribution with predilection for long bones of lower extremities.
This can mimic infectious
osteomyelitis or malignant tumors in children. During exacerbations, high CRP and ESR are
found in more than half patients. However, it is not usual to find objective
anemia and Rheumatoid factor is negative. Only ten percent of patients are
positive for HLA-B27[3]. Comorbid conditions
found in CRMO may include spondyloarthropathy, psoriatic arthritis
as well as Inflammatory Bowel Disease (Crohn’s
disease or ulcerative colitis). Comorbid conditions can be absent in the onset
of the disease and
appear after 1 to 5 years of evolution[4,5].
SAPHO
is also characterized by episodic recurrent bone pain due to non-bacterial osteitis [6]. The most commonly affected bones are located
in the chest wall [7]. The osteitis can be unifocal or multifocal and
asymmetric. One of the distinguishing SAPHO features is the finding of severe
skin manifestations. Severe scarring acne, psoriasis or palmoplantar
pustulosis are commonly present on examination. SAPHO
syndrome has an older age of
presentation. The onset is usually at 30 years(12-65
years) [6,7]. Moreover, SAPHO has predilection for different bones.
In
our case most of the lesions were located in long bones and the chest wall was
free. The diagnosis of CRMO was more plausible.
In
all cases, both CRMO and SAPHO should be diagnosis of exclusion. It is always
mandatory to rule out infection, malignancy, and systemic autoimmune diseases. The
diagnosis is usually made on both clinical and radiological arguments. The MRI
whole body could be useful. It detects infra-clinic osteitis
sites. The cartography of the lesions could evoke the diagnosis [8]. The
treatment is almost always based non-steroidal anti-inflammatory molecules for
mild cases. Otherwise corticosteroids and interleukin-1 receptor antagonist
(IL-1Ra) may be required. The indications for surgery are rare [9,10].
Conflict
of Interest: None
Acknowledgments
We
thank Professor Mouna Bouaziz-Cheli
and Professor Noureddine Bouzouaya
for collaborating in the management of this patient.
This
report does not contain any personal information that could lead to the
identification of the patient. A parent’s consent was obtained.
References
[1]
Hofmann SR, Kapplusch F, Girschick
HJ, Morbach H, Pablik J,Ferguson PJ et al.
Chronic Recurrent Multifocal Osteomyelitis (CRMO): Presentation, Pathogenesis,
and Treatment. Curr Osteoporos
Rep. 2017;15:542-54.
[2]
Roderick MR, Shah R, Rogers V, Finn A, Ramanan AV.
Chronic recurrent multifocal osteomyelitis (CRMO) - advancing
the diagnosis. Pediatr Rheumatol
Online J. 2016;14:47.
[3]
Hofmann SR, Kubasch AS, Range U, Laass MW
, Morbach H , Girschick HJ,
et al. Serum biomarkers for the diagnosis and monitoring of chronic recurrent
multifocal osteomyelitis (CRMO). Rheumatol Int. 2016;36:769-79.
[4]
Jelušić M, Čekada
N, Frković M, Potočki
K, Skerlev M, Murat-Sušić
S, et al. Chronic Recurrent Multifocal Osteomyelitis (CRMO) and Synovitis Acne Pustulosis
Hyperostosis Osteitis (SAPHO) Syndrome - Two
Presentations of the Same Disease? Acta Dermatovenerol Croat. 2018;26:212-19.
[5]
Yamashita
K, Calderaro C, Labianca L,
Gajaseni P, Weinstein SL.
Chronic recurrent multifocal osteomyelitis (CRMO) involving spine: A case
report and literature review. J Orthop Sci. 2018;S0949-2658(18)30168-4.
[6]
Firinu D, Garcia-Larsen V, Manconi PE, Del Giacco SR. SAPHO
Syndrome: Current Developments and Approaches to Clinical Treatment. Curr Rheumatol Rep. 2016;18:35. [7] Cianci F, Zoli A, Gremese E, Ferraccioli G. Clinical heterogeneity of SAPHO syndrome:
challenging diagnose and treatment. Clin Rheumatol. 2017;36:2151-58.
[8]
Jurik AG, Klicman RF, Simoni P, Robinson P, Teh J.
SAPHO and CRMO: The Value of Imaging. Semin Musculoskelet Radiol.
2018;22:207-24.
[9] Daoussis D, Konstantopoulou G, Kraniotis
P, Sakkas L, Liossis SN. Biologics
in SAPHO syndrome: A systematic review. Semin Arthritis Rheum. 2019;48:618-25.
[10]
Vargas
Pérez M, Sevilla Pérez B. SAPHO syndrome in
childhood. A case report. Reumatol
Clin. 2018;14:109-112.