Full Text Article Open
Access 
Original Article
Traumatic versus non traumatic
spinal cord injury:
Characteristics and functional outcome in a Tunisian rehabilitation centre
Gaddour Mariem 1,2*, Ouannes Walid 1,2, Frioui Samia 1,2, Salah Sana 3, Khachnaoui Fayçal 1,2, Jemni Sonia
1,2.
|
1: Physical medicine and rehabilitation Department, university hospital Sahloul, Sousse, Tunisia.
2: College
of medicine Sousse Tunisia
3: Physical medicine and rehabilitation Department, university hospital Fattouma Bourguiba, Monastir,
Tunisia
*Corresponding author Correspondence to: gadmariem@gmail.com Publication data: Submitted: February 5, 2018
Accepted: April 24, 2018
Available Online: June
22,2018
This article was subject to full peer- review.
|
Abstract
|
|
Background:
Understanding of the underlying mechanisms of Spinal
cord injury (SCI) would help in the development of treatment strategies and enhance
neurological recovery.
Aim:
The aim of this study was to describe clinical and demographic data of SCI in a physical medicine department and to compare neurological and functional outcome in Traumatic Spinal
Cord Injury group (TSCI) and Non Traumatic Spinal Cord Injury
group (NTSCI) during
two years of follow
up.
Materials and methods:
This study was conducted in a physical medicine and rehabilitation department of a tertiary hospital (January 2008-December 2014).
Medical records of 177 patients with spinal
cord injury (SCI) were reviewed. Two groups
were defined: traumatic (TSCI) and non-traumatic (NTSCI) spinal cord injury. Characteristics and functional outcome
were analyzed and compared.
Results:
Patients of NT group
were significantly older.
Most of injuries in both groups had a cervical level. ASIA scale scores
and MIF scales
were significantly higher
in NT group at admission and after
two years of follow
up. The impairment was more remarkable in this group.
Conclusions:
Our study suggests that non traumatic SCI represent a considerable proportion of SCI
rehabilitation admissions. Although different characteristics and injury patterns, functional outcomes maybe comparable to traumatic SCI.
Key words:
spinal cord injury, epidemiology, etiology, rehabilitation
|
Introduction:
Spinal cord injury (SCI) is an event that results in a disturbance to normal sensory, motor, or autonomic nervous function. It may also lead to several disorders
of organ systems, such as respiratory, joint, and urinary
system. SCI usually
affects also the patient’s psychological, and social well-being. The annual global incidence of SCI is 10.4 to 83 cases per million [1]. It may arise from traumatic and non- traumatic causes.
In both types of injury,
the damage suffered
can progress unpredictably. The management of severe
cases is difficult due to the lack of guidelines and
the
high cost of the consensual procedures. Implementing an appropriate prevention strategy require
an established knowledge on injury mechanisms, disease pathophysiology, and disability characteristics [2].
Patients and
methods:
This is a retrospective study (2088-2014) conducted in the physical medicine
and rehabilitation department of Sahloul university hospital, Sousse, Tunisia.
Medical records of patients
with SCI admitted were reviewed. Patients
were divided into two groups: T group (for TSCI) and NT group (for NTSCI). Patients diagnosed
with traumatic Cauda equina syndrome were excluded
from group T. Cases of Myelopathy cervicarthrosis majored by a trauma were not included
in group NT. The variables
studied were associated with the social demographic profile of patients (age, gender,
marital status, personal income,
social care, occupation and comorbidities). In addition, the cause, type and level of spine injury were specified
in the physical
examination. Neurological levels of SCI were classified using the American
Spinal Injury Association Impairment
Scale (AIS)(Appendix1). Functional status at admission and after two years of follow up was assessed
by functional independence measure (FIM) (Appendix 2). Concomitant injuries, length of stay (LOS) and different treatment
options were recorded.
Recordings were made at the time of admission in rehabilitation department as well as after two years.
Statistical analysis was performed using SPSS software (version
17.0). Descriptive statistics were used to represent data as average, range, median and percentages. Ordinal data were expressed as medians, inter-quartile ranges,
and percentages. For this normal distribution, Chi-square
(χ2) tests of comparison was applied. Independent t-tests were used to compare parametric variables. A p value < 0.05 was considered as significant.
Results:
During the study,
177 patients with SCI were included. Defined groups were: TSCI (T group; n
=108) and NTSC (NT group; n=69). Sociodemographic data is represented in Table1. Patients of NT group were significantly older (p<0.001). however sociodemographic profiles of the two groups were comparable (p>0.05).
Road traffic accidents (RTA) were the main cause of TSCI. Main concomitant injuries observed were brain injuries in 19 patients
(17.6%), rib fracture in 13 cases (12.0%) and pelvis fracture in 9.3 % of cases.
Regarding NT group, degenerative disease
was the main cause of NTSCI including discal hernia and myelopathy in 30.4 % and 20.1% respectively. Mechanisms of SCI in both groups are summarized in table 2.
Regarding baseline evaluation, the cervical level was the most frequently affected region
in both groups. AIS scores were significantly higher in NT group at admission (p<0.001). In T group, most of patients were AIS A. However, in NT group, most of lesions were classified as AIS D. Thirteen patients of T group
were diagnosed with conus medullaris versus
5 cases in NT group.
Patients with TSCI showed
a significant lower functional status at admission than NT group (96.0%
vs 76% of T and NT group respectively had FIM scores lower than 100/126). Details of baseline evaluation are represented in table 3.
Table1: SCI Sociodemographic characteristics
Table2: Spinal cord injury mechanisms
Regarding
the operative management; surgical decompression was earlier in T group.
Medical management of SCI depended on the etiology. It included antibiotics
(infectious spondylodiscitis), anti-tubercular agents and corticosteroids
(tuberculosis), embolization, chemotherapy, radiation (neoplastic diseases).
Regarding urinary dysfunctions, treatment strategies were adapted to bladder
disorder types.
Treatment
of overactive bladder was based on anticholinergic drugs and self-intermittent
catheterization (76.9% and 44.9% of T and NT group, respectively). Five
patients in T group had suprapubic catheter for urinary retention in case of
urethral trauma or penile sores.
Table3: Baseline
evaluation
Requirement of assistance devices was significantly higher in T group
(92.6% versus 62.3% in NT group: P <0.001).
Readmissions in rehabilitation department characteristics were analyzed
and compared between the two groups. The rate of readmission was significantly
higher in T group (33.6% of T group, 12.8 % of NT group: P=0.01).
Characteristics of SCI readmissions are summarized in table 4.
Table4: Characteristics of readmissions in SCI
|
Readmission
|
T
|
NT
|
|
%
|
33.6
|
12.9
|
|
Average time to readmission
|
432
|
404
|
|
Mean inpatient days
|
19
|
7
|
|
FIM
score
|
73/126
|
95/126
|
|
% Scheduled /complications
|
55.6/44.4
|
70 /30
|
A variety of complications was diagnosed
during the follow up of patients
with clear difference between the
two groups. In fact, all types of complications were significantly more frequent
in T group.
However, the comparative study could not be independent from postoperative courses factors.
Managed complications are detailed
in table 5.
Table 5: Major complications
ASIA scale scores
and MIF scales were significantly higher in NT group at admission
and after two years of follow
up as compare
with T group. Details
of final evaluation are represented in table 6.
Table 6: final
assessment
On the basis of the present findings neurological and functional impairment was higher in T group as compare
with NT group, not only at admission in rehabilitation department, but also after two years of follow.
Discussion:

 Spinal cord injury is a devastating condition. In addition
to organic and psychological disorders; SCI management represents substantial financial challenge
on patients and society [3,4]. A comprehensive study of the leading
factors and the pathological behaviour of SCI has simplified the management and improved the prognosis. Trauma contributes to the largest
proportion of SCI. The demographic data, etiology,
and functional outcome have been well codified for traumatic
SCI in the previous published
literature [5]. Male predominance is usually noticed for traumatic SCI. In our study,
patients in T group
were male in 71.3% of cases.
This was concordant with earlier studies results [5,6]. Regarding
non-traumatic SCI; Citterio and al have also reported a male predominance (58%) [7]. However,
most of the other authors found a female predominance independent from the etiology
[6-8]. Traumatic
SCI affect more young adults. In our study, mean age of patients in T group
was 34 years (21-30). However a remarkable increase of traumatic
SCI incidence is noticed in older population [9,10].
This can be explained
by the progress
of demographic assessment and a higher accident
rate beyond the age of 65 [11].
Spinal cord injury is a devastating condition. In addition
to organic and psychological disorders; SCI management represents substantial financial challenge
on patients and society [3,4]. A comprehensive study of the leading
factors and the pathological behaviour of SCI has simplified the management and improved the prognosis. Trauma contributes to the largest
proportion of SCI. The demographic data, etiology,
and functional outcome have been well codified for traumatic
SCI in the previous published
literature [5]. Male predominance is usually noticed for traumatic SCI. In our study,
patients in T group
were male in 71.3% of cases.
This was concordant with earlier studies results [5,6]. Regarding
non-traumatic SCI; Citterio and al have also reported a male predominance (58%) [7]. However,
most of the other authors found a female predominance independent from the etiology
[6-8]. Traumatic
SCI affect more young adults. In our study, mean age of patients in T group
was 34 years (21-30). However a remarkable increase of traumatic
SCI incidence is noticed in older population [9,10].
This can be explained
by the progress
of demographic assessment and a higher accident
rate beyond the age of 65 [11].
In our study, patients of NT group were significantly older (49 years vs 34 years). This finding is widely described
in the literature [4,7,11].
Moutquin and al found a significant higher rate of associated comorbidities in non-traumatic SCI [12]. That was the case of diabetes (6%), cancer (57%) and chronic obstructive pulmonary
disease (2%).
As previously reported; the most two common causes of traumatic
SCI are Road traffic accidents and falls (respective incidence are 48.1% and 25.0%) [11,12,13]. However, in non-traumatic SCI; degenerative diseases remain the most common cause (50.7%)
[13].
Most of injuries in both the groups are located in a cervical level. Gupta and al reported most frequent thoracic and lumber
injuries especially in non- traumatic
SCI [14].
Regarding
AIS scale at admission, we found a significant difference between
the two groups. The majority
of the T group patients (61.1%) presented with an AIS "A", however in the NT group most of patient’s
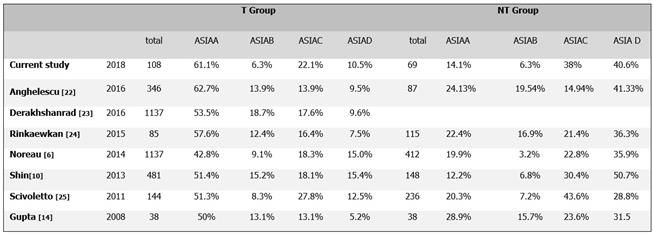
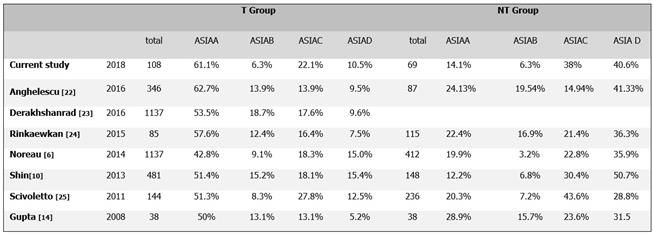
AIS were "C" or "D". Our results are similar to those described in the literature. Table 6 summarizes recent works dealing with this subject.
Recent
epidemiological studies
reported that patients diagnosed
with traumatic SCI have more complete lesions. In our study, comparable findings could be seen (61.1% of the T group had complete lesions compared to 11.5% in the NT group, P
<0.001). This can be explained by the high velocity and sudden
mechanisms in traumatic injuries [12,14].
Length of stay in rehabilitation department is considered as indicator
in the outcome assessment. A significant difference was found between the groups in our study.
Patients
in NT group had a shorter rehabilitation than those in T group (24 days vs 40 days). Several
factors may contribute to a longer rehabilitation for traumatic SCI patients. These factors include the treatment
of concomitant injuries and the management of non-specific complications which are more frequently observed [15].
 Even consensual and well codified;
the management of SCI is still difficult. A multidisciplinary team management approach is mandatory in the rehabilitation of SCI. In addition to the managing
physicians; the team should include by a physiotherapist, a dietician, and a psychologist. Training and education
of the patient’s family improve
always the treatment
outcome [16].
Even consensual and well codified;
the management of SCI is still difficult. A multidisciplinary team management approach is mandatory in the rehabilitation of SCI. In addition to the managing
physicians; the team should include by a physiotherapist, a dietician, and a psychologist. Training and education
of the patient’s family improve
always the treatment
outcome [16].
Table 6: Literature review
Early inpatient
rehabilitation program aims to teach the patient
the daily tasks achievement. This may include the wheelchair use skills, bowel and bladder management, and skin care. The prevention and the management of late complications is considerable part of the treatment.
Urinary
tract disorders, pressure ulcers,
deep venous thrombosis, spasticity, and depression are frequent
and delay patient autonomy recuperation [17].
 The use of specific
scores simplify the assessment and make from physical examination findings a measurable entity that could be followed up. In our study; FIM scores
at the time of admission and
after two years were recorded
and used as functional outcome measurement
tool. The mean MIF was 52.7/126 in T group versus
78 in NT group (P<0.001). The significant difference in traumatic SCI patients
is attested by all the authors
and highlights the severity of pathological lesions as well as the delayed healing
in these cases. [18-20]. According to Ditunno; most asked questions asked by patients
and their relatives are related to motility function “Will i be able to walk?” [20]. Social
and psychological assistance is capital
during the walking recovery period
[21].
The use of specific
scores simplify the assessment and make from physical examination findings a measurable entity that could be followed up. In our study; FIM scores
at the time of admission and
after two years were recorded
and used as functional outcome measurement
tool. The mean MIF was 52.7/126 in T group versus
78 in NT group (P<0.001). The significant difference in traumatic SCI patients
is attested by all the authors
and highlights the severity of pathological lesions as well as the delayed healing
in these cases. [18-20]. According to Ditunno; most asked questions asked by patients
and their relatives are related to motility function “Will i be able to walk?” [20]. Social
and psychological assistance is capital
during the walking recovery period
[21].
In our study, 38.9% of T group and 89.9% of NT group were walkers.
These patients were initially classified AIS “C” or “D”. Actually
the chance of walking recovery after a SCI can be predicted from the admission time. Patients with complete
lesions have very limited chance for full recovery.
The prognosis is better for partial lesions in young patients and in the absence
of severe associated comorbidity or late complications. The prevention and early diagnosis
improve the treatment results is both types of SCI [22].
The WHO recommended three levels prevention strategy
to improve functional prognosis
of SCI. Primary consist
in the control of the leading factors such as road traffic accident for trauma SCI. Secondary
prevention aims to ensure
an early diagnosis of the injury and an efficient
management (complete initial neurological examination, quick screening and early decompressive surgery).
Tertiary
prevention aims to minimize
durable side effects and to improve
patient’s re-integration [23-25].
Conclusions:
Understanding of the underlying mechanisms and the control of the leadings factors would help in the development of SCI treatment strategies and enhance neurological recovery.
 This report corroborates many previously evident
facts; especially the difficulty of the management of traumatic
cases. However it showed a comparable treatment results in both types of lesions
in an area of very high accidents
rate. The rehabilitation is as important
as the first given care. It should be driven in a well codified scientific way to ensure a maximum of recuperation. A larger study may allow to avoid statistical bias and give more objective
results.
This report corroborates many previously evident
facts; especially the difficulty of the management of traumatic
cases. However it showed a comparable treatment results in both types of lesions
in an area of very high accidents
rate. The rehabilitation is as important
as the first given care. It should be driven in a well codified scientific way to ensure a maximum of recuperation. A larger study may allow to avoid statistical bias and give more objective
results.
Conflict of interest: none
[1] Osterthun, R, Post M W M, Van Asbeck F W A. Characteristics, Length of Stay and Functional Outcome of Patients with Spinal Cord Injury in Dutch and Flemish Rehabilitation Centres. Spinal Cord.2009; 47(4): 339-44.
[2] Guilcher SJ, Munce SE, Couris CM, Fung K, Craven BC, Verrier M, Jaglal SB. Health care utilization in non- traumatic and traumatic spinal cord injury: A population- based study. Spinal Cord.2010 ;48(1):
45-50.
[3] St Andre JR, Smith BM, Stroupe
KT, Burns
SP,
Evans CT, Ripley DC et al. A comparison of costs and health care utilization for veterans with traumatic
and nontraumatic spinal cord injury.
Top Spinal Cord Inj Rehabil. 2011;16(4):27-42.
[4] Yang R, Guo L, Wang P, Huang L, Tang Y, Wang W, et al. Epidemiology of spinal cord injuries
and risk factors for complete injuries in Guangdong, China: a retrospective study. PLoS One. 2014; 9(1): e84733.
[5] Zárate-Kalfópulos, B, Jiménez-González A, Reyes-
Sánchez R, Robles-Ortiz R, Cabrera-Aldana E, Rosales-
Olivarez L. Demographic and clinical characteristics of patients
with spinal cord injury: a single hospital-based study. Spinal Cord.2016; 54(11):
1016-19.
[6] Noreau L, Noonan V, Cobb J, Leblond J, Dumont F. Spinal Cord Injury Community Survey: A national, comprehensive study to portray the lives of Canadians with spinal
cord injury. Topics
in Spinal Cord Injury Rehabilitation.2014; 20(4):
249-64.
[7] Citterio A, Franceschini M, L Spizzichino L, Reggio A, Rossi B, Stampacchia G. Nontraumatic spinal cord injury: An Italian
Survey. Archives of Physical
Medicine and Rehabilitation.2004; 85(9): 1483-87.
[8] New P W. Functional outcomes and disability after nontraumatic spinal cord injury rehabilitation: Results from a retrospective
study. Archives of Physical Medicine and Rehabilitation.2005; 86(2): 250-61.
[9] Shihao Z, Wadhwa R, Haydel J, Toms J, Johnson
K, Guthikonda B. Spine and Spinal Cord Trauma. Neurologic Clinics.2013; 31(1):
183-206.
[10] Shin, J C, Kim DH, Yu SJ, Hea Eun Yang HE, Yoon SY. Epidemiologic Change of Patients with spinal
cord injury. Annals of Rehabilitation Medicine.2013; 37(1): 50-56.
[11] McKinley WO, Seel RT, Gadi RK, Tewksbury MA. Nontraumatic vs. traumatic spinal cord injury. Am J Phys Med Rehabil
.2001 ; 80 : 693-99.
[12] Moutquin
J M, Larouche K, Mayot M H, Rossignol
M. Lésions médullaires traumatiques et non-traumatiques : analyse comparative des caractéristiques et de l’organisation des soins et services de réadaptation au Québec : l’Institut national d’excellence en santé et en services sociaux ; Fev 2013. Rapport ETMIS.
2013 ;9(1).
[13] Kay E, Deutsch
A, Chen D, Larry Manheim L, Rowles
D. Effects of etiology on inpatient
rehabilitation outcomes
in 65- to 74-year-old patients with incomplete paraplegia from a nontraumatic spinal cord injury.
PM&R.2010; 2(6): 504-13.
[14] Gupta A, Taly AB, Srivastava A, Vishal S, Murali T. Traumatic vs non-traumatic spinal cord lesions: Comparison of neurological and functional outcome after in-patient rehabilitation. Spinal Cord.2008; 46(7): 482-87.
[15] Majdan M, Brazinova
A, Mauritz W. Epidemiology of traumatic
spinal cord injuries
in Austria 2002-2012. Eur Spine J.2015;
25: 62-73.
[16] Bauchet L, Lonjon N, Perrin FE, Gilbert C, Privat A, Fatta C. Strategies for spinal cord repair after injury: A review of the literature and information. Annals of Physical and Rehabilitation Medicine.2009; 52(4):
330-51.
[17] Perrouin-Verbe B. Rehabilitation of spinal
cord injury patients.
Bulletin De l’Academie Nationale De Medecine.2005; 189(6):
1159-74.
[18] Kemal N, Yazmalar L, Sah V, Aydin A, Ones K. Rehabilitation of Spinal Cord Injuries. Worl J Ortho.2015; 6(1): 8-16.
[19] Lofvenmark I, Norrbrink
C, Nilsson-Wikmar L, Hultling C, Chakamdinakira S, Hasselberg M. Traumatic spinal cord injury in
Botswana: characteristics, aetiology and mortality. Spinal
Cord. 2015; 53: 150-54.
[20] Ditunno JF. Predicting recovery after spinal cord injury: A rehabilitation imperative. Archives of Physical Medicine and Rehabilitation.1999; 80(4):
361-64.
[21] Scivoletto G, Tamburella F, Laurenza L, Torre M, Molinari M. Who is going to walk? A review of the factors
influencing walking recovery after spinal cord injury. Front Hum Neurosci.2014; 8:141.
[22] Anghelescu A, Onose LV,
Popescu C, Andone I, Octaviana DC, Magdoiu AM, et al. Evolution of traumatic
spinal cord injury in patients with ankylosing spondylitis, in a Romanian
rehabilitation clinic. Spinal Cord Ser Cases. 2016; 2:16001.
[23] Derakhshanrad N, Yekaninejad
M, Vosoughi F, Fazel FS, Saberi H.
Epidemiological study of traumatic spinal cord injuries: experience from a
specialized spine center in Iran. Spinal cord. 2016; 54:901-7.
[24] Rinkaewkan P,
Kuptniratsaikul V. The effectiveness of inpatients rehabilitation for spinal
cord patients in Siriraj Hospital. Spinal Cord.2015; 53(8): 591-97.
[25] Scivoletto G, FarchiS,
Laurenza L,Molinari M. Traumatic and non-traumatic spinal cord lesions: An
Italian comparison of neurological and functional outcomes. Spinal Cord.2011;
49(3): 391-96.
Appendix 1

Appendix 2
Citation: Gaddour M, Ouannes W, Frioui S, Salah
S, Khachnaoui F, Jemni S. Traumatic versus non traumatic spinal cord injury: Characteristics and functional outcome in a
Tunisian rehabilitation center. Junior
Medical Research. 2018; 1(2):12-21. Gaddour
et al
© All rights are reserved. Submit your manuscript: www.jmedicalresearch.com