Full Text Article Open
Access 
Case report
Aneurysmal Bone Cyst of D2 in a Child complicated with paraplegia.
Jlidi Mohamed1,4, Triki Ramy1,4, Jlalia Zied1,4*, Riahi Hend2,4, Fareh Klibi Faten3,4, Daghfous Samir1,4.
|
1
Department of pediatric orthopedics, Kassab
Institute Tunis,
Tunisia
2
Department of radiology, Kassab
Institute Tunis,
Tunisia
3
Department of pathology, Kassab
Institute Tunis,
Tunisia
4
College
of medicine Tunis Tunisia
*Corresponding author Correspondence to: Jlalia.zied@gmail.com Publication data: Submitted: May
9,2018
Accepted: June
10,2018 Available
Online: June 22,2018
This article was subject
to full peer-review.
|
Abstract
|
|
Aneurysmal bone cysts (ABCs) are
benign osteolytic lesion
representing
15% of all primary spine
tumors. We report a case of a 9-year-old girl who had an ABCs localized in D2.
Symptoms involved back
pain and paraplegia. Radiology investigations
showed osteolysis of D2 and
anterolisthesis of C7 and D1.
The patient had a posterior decompression and laminectomy of D2, D3 and D4 without
neurological improvement. Surgical biopsy confirmed the diagnosis.
Computed tomography scan showed
tumor remnants. An embolization of the tumor and an anterior liberation associated with bone graft were performed.
The result was a spectacular neurological improvement with disappearing of all neurological symptoms. Radiology investigations follow up showed only spine
instability but no residual tumor.
Key words: Tumor; Cyst; Bone;
Spine.
|
Introduction:
Aneurysmal bone cysts (ABCs)
are benign and locally aggressive osteolytic lesions. They represent 1.4% of primary bone tumors; 9.1% of all bone tumors; and only 15% of primary
spine tumors [1]. These lesions occur either in thoraco-lumbar or cervical spine.
These locations are problematic due to the frequency
of spine instability. The reconstructive surgery is always challenging [2].
Case presentation:
Our case is a 9-year-old girl with no previous
medical history. She first presented with back
pain and progressive paraplegia. There was no history of trauma or fever. Physical examination showed neck stiffness, flaccid paraplegia and abolition
of tendon reflexes.
There was no sensory neither
sphincterian disorders.
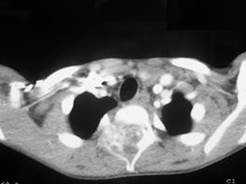
 The X-ray
showed osteolysis of D2
and anterolisthesis of C7 and D1. The CT scan showed an osteolytic lesion
in the posterior arch of D2 vertebrae
(Figure 1). The lesion was compressing the
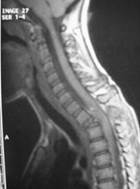
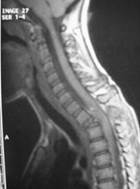
spinal cord. The MRI showed hypersignal of the vertebrae
D2 in T1 and T2 weighted
sequences with vascular enhancement and medullary compression (Figure
2).
The X-ray
showed osteolysis of D2
and anterolisthesis of C7 and D1. The CT scan showed an osteolytic lesion
in the posterior arch of D2 vertebrae
(Figure 1). The lesion was compressing the
spinal cord. The MRI showed hypersignal of the vertebrae
D2 in T1 and T2 weighted
sequences with vascular enhancement and medullary compression (Figure
2).
The patient first had a posterior decompression and laminectomy of D2, D3 and D4, stabilized by a halo cast. A surgical
biopsy was also performed, and it was in favor of ABC (Figure 3).
There was no neurological improvement after the surgery. Spasticity of lower appeared one month later. A CT scan showed tumor remnants
in the medullar cavity
(Figure 4). An embolization of the tumor was performed
(figure 5), associated with anterior
liberation, bone graft and stabilization with halo cast for three months.
6 months later, the neurological defect has disappeared. The muscular
testing was normal.
CT scan follow
up showed that there is no recurrence of the tumor (Figure 6). At 9 years after the surgery,
the patient is living a normal life and has no complaints. No recurrence of the tumor was observed.
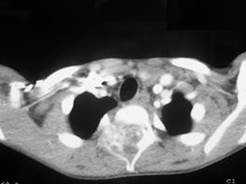
Figure 1: CT axial
images show an expansive and lytic lesion in
the vertebral body, right pedicle, transverse and spinous
process of D2 which
enhance after
contrast injection with moderate canal compromise

(a)

(b)
Figure 2: a) T1, T2 tumoral appearances b) T2 with
injection of gadolinium contrast: hypersignal of the vertebrae D2 in T1 and T2 weighted
sequences with vascular enhancement and medullary compression
Figure 3: Histological study a: cavities separated by septa of various
thickness. These cavities
were filled with red blood cells. b: Thin osteoid
hyaline bands close of the borders of the cavities
Figure 4: Tumor remnants
in the medullar
cavity
Figure 5: Pre-operative embolization of the tumor Figure 6: follow
up CT scan at 6 months
Discussion:
ABC was first considered as a variety of giant cell tumors,
then as an isolated tumor-like bone dystrophy. But its real nature is still unknown. ABC was first described
in 1942 by Jaffe and Lichtenstein [3]. This terminology was, since then, world widely
used, even ABCs are neither cysts, nor aneurysms. It is a tumor-like lesion and can be individualized in two forms: primitive ABC, which is an independent entity (70% of the cases), and secondary
ABC (30% of the cases),
which is a reactional and developed
on a preexisting lesion
[4].
Pathogenic mechanisms
of ABC are still discussable. Recent
researches, particularly genetic
and immuno-histochemical, are tending to prove that ABC is more a tumor than a tumor-like lesion. However, pathogenesis of ABC is probably multifactorial. In an epidemiological multicentric study about 411 children with primitive
ABC, femur (22%), tibia (17%), spine (15%), humerus (10%), pelvis (9%) and fibula (9%) were the most frequent localizations [5]. Lumbar
region is the most frequently affected in the spine.
ABC is first found in the posterior arc (40% of unique lesions),
then fills the vertebral body in the front side via the pedicle,
adjacent vertebrae
in the up and downside via the articular processes, and the ribs laterally. Isolated localization in the body of the vertebrae is very rare [6]. ABC
can present in a form
of stiff and painful
scoliosis, with an important functional disability. A neurological syndrome
is found in 50% of the cases. Neurological signs, like radicular
compression, are either progressive due to the growth of the size of the tumor, or brutal due to the damage caused in the vertebral body. X-rays and CT scan findings depend on the stage of ABC. During the osteolytic stage,
radiological images are usually zones of eccentric bone depletion. The active growth stage shows a sub-periosteal eruption. Healing
stage is characterized by progressive calcification and ossification of the cyst [7].
MRI can localize the lesion
and its extension, confirm its sub-periosteal situation and analyze
the surrounding vessels and noble structures. Some images
are very revealing, like a well-limited expansive bone lesion,
a decrease
of signal in T1 associated with increase
of the signal in T2 (liquid
compound), a peripheral border
of low signal enhanced by the injection of gadolinium, multiple small cavities confined by septa and the presence of liquid-liquid levels.
Association of X-ray and MRI is helpful
for the diagnosis of ABC, but biopsy is mandatory before
the treatment for histological confirmation [8].
Selective arterial embolization, used as the only treatment, or during
the pre-operative phase (an uncontrollable bleeding in this region can be fatal) is admitted by all the authors.
It is widely used when the ABC affects the spine and the pelvis where
we can’t use a pneumatic tourniquet. Complications as ischemia
of neurological structures or other organs are possible
[9].
If surgery is indicated, it must fulfill
three obligations: the complete excision of the tumor, decompression of the spinal cord and reconstruction and stabilization of the spine. It is essential, especially in this localization, to treat the lesion in only one surgical
procedure. further surgeries are challenging and always complicated [10].
Surgical curettage is the most appropriated treatment for ABC of the spine. It consists
in accessing the cyst via a window,
performing a careful
curettage of its cavity and excising its lining. We can combine this technique
with bone graft. Most of the recurrences occur during the first months after the treatment (3 to 6 months).
There are usually
less chances of recurrence in the vertebral localizations [11,12].
Conclusion:
ABCs are benign
and rare tumors of the child. A stiff and painful back is the most frequent warning sign. This tumor can be severe when it is localized
in the spine because of its neurological risks. Surgical treatment is essential
when neurological symptoms are present.
Conflict of interest: none
References:
[1]Burch S, Hu S, Berven S. Aneurysmal bone cysts of the spine. Neurosurg Clin N Am.2008;
19: 41-47.
[2]Mascard E, Gomez-Brouchet A, Lambot
K. Bone cysts: unicameral and aneurysmal bone cyst. Orthop Traumatol Surg Res. 2015 ;101(1): S119-27.
[3]Jaffe HL, Lichtenstein L: Solitary unicameral bone cysts with emphasis
on the roentgen
picture, the pathologic appearance and the pathogenesis. Arch Surg. 1942; 44: 1004-25.
[4]Tsagozis P, Brosj O. Current
Strategies for the Treatment of Aneurysmal Bone Cysts. Orthop
Rev. 2015 28 ;7(4) :106-10.
[5]Cottalorda J, Kohler R, Sales De Gauzy J, Chotel F, Mazda K, Lefort G, et al: Epidemiology of aneurysmal bone cysts in children: a multicenter study and literature review. J Pediatr
Orthop B, 2004, 13, 389-94.
[6]Zileli M, Isik HS, Ogut FE, Is M, Cagli S, Calli C. Aneurysmal bone cysts of the spine. Eur Spine J. 2013 ;22 (3):593-601.
[7]Riahi H, Mechri M, Barsaoui
M, Bouaziz M, Vanhoenacker F, Ladeb M. Imaging of Benign Tumors of the Osseous
Spine. Journal of the Belgian Society of Radiology. 2018; 102(1): 1-11.
[8]Chan MS, Wong YC, Yuen MK, Lam D. Spinal aneurysmal bone cyst causing acute cord compression without vertebral
collapse: CT and MRI findings.
Pediatr Radiol. 2002 ;32(8):601-4.
[9]Terzi S, Gasbarrini A, Fuiano M, Barbanti Brodano G, Ghermandi R; Bandiera
S; et L. Efficacy
and Safety of Selective
Arterial Embolization in the Treatment
of Aneurysmal Bone Cyst of the Mobile Spine: A Retrospective Observational Study. Spine.2017; 42(15):1130-38.
[10]Park HY, Yang SK, Sheppard WL, Hegde V, Zoller SD, Nelson SD, et al. Current management
of aneurysmal bone cysts. Curr Rev Musculoskelet Med. 2016;
9(4): 435-44.
[11]Hauschild O, Ludemann
M, Engelhardt M, Baumhoer D, Baumann T, Elger T, et al. Aneurysmal bone cyst (ABC): treatment options and proposal of a follow-up
regime. Acta Orthop
belg. 2016; 82(3):474-83.
[12]Ulici A, Nahoi C, Carp M, Fodor I,Dinu C. Surgical
Treatment of an Aneurysmal Bone Cyst with
Avascular Bone Graft. Chirurgia
(Bucur). 2017 ;112(2):172-77.
Citation:
Jlidi M, Triki R, Jlalia Z, Riahi H, Fareh Klibi F, Daghfous S. Junior Medical
Research. 2018; 1(2):26-30. Jlidi et al © All rights are reserved. Submit
your manuscript: www.jmedicalresearch.com