
Full Text Article Open
Access 
Original article
Evaluation of the circadian fluctuations of intraocular pressure
and ocular perfusion
pressure in different types of glaucoma
Giambene Barbara*
|
*Corresponding author Correspondence to: barbargiambene@virgilio.it Publication data: Submitted: December
14,2017 Accepted: December 27,2017
Available Online: January 31,2018 This article was subject
to full
peer-review. |
Abstract |
Background:
Glaucoma is a frequent leading cause of blindness. Objective evidence showed that it can be secondary to optic
nerve head hypoperfusion and autonomic dysfunction, not only
to ocular hypertension. This makes
the assessment of ocular
blood flow a crucial
step in the management of this disease. Aim:
To investigate the circadian fluctuations of the intraocular pressure (IOP)
and of the mean
ocular perfusion pressure (mOPP) in patients with different types of glaucoma. Materials and methods:
Sixty-five eyes of 65 glaucoma patients, managed
in the Ophthalmology Department of the Careggi University Hospital, Firenze, Italy
(2012-2014). Among these eyes,
22 had normotensive glaucoma (NTG), 21 hypertensive glaucoma (HTG), and 22 exfoliative glaucoma (XTG). The IOP was measured by Goldmann tonometry and the blood pressure, both systolic (sBP) and diastolic (dBP), by
Riva-Rocci sphygmomanometry, at
three time
points (8am,
2pm, 8pm). The mOPP was then calculated according to the formula mOPP = [2/3 (2/3 dBP + 1/3sBP)
- IOP]. Results:
The
fluctuations of IOP and
mOPP were statistically significant in all the studied eyes (p<0.001 for all the comparisons). Both IOP and mOPP showed
significantly larger
fluctuations in the XFG eyes
than in the NTG and HTG ones (p<0.001 for IOP and p=0.001 for mOPP). Conclusions:
In our study, the mOPP had larger circadian fluctuations in eyes with XFG than in those with
NTG and HTG. This parameter deserves to be assessed in all types of glaucoma. Key words: Glaucoma, intraocular pressure, mean ocular
perfusion pressure. |
Introduction:
Glaucoma is currently defined as a chronic progressive optic neuropathy with typical anatomical and clinical features and consequent visual impairment. Other than ocular hypertension, optic nerve head hypoperfusion and autonomic dysfunction are the most relevant physio-pathologic risk factors [1].
The aim of this study is to assess the circadian fluctuations of the intraocular pressure (IOP) and of the mean ocular perfusion pressure (mOPP) in patients with different types of glaucoma.
Materials and methods:
Sixty-five eyes of sixty-five glaucoma patients, referred to the Ophthalmology Department of the Careggi University Hospital, Firenze, Italy in the period 2012-2014 were included in this retrospective study, approved by the local ethic committee. The eyes were divided in three groups: normotensive glaucoma (NTG, n=22), hypertensive glaucoma (HTG, n=21) and exfoliative glaucoma (XFG, n=22). All the selected eyes had normal corneal thickness values and were matched for severity of disease (moderate, GSS 1L-2L) and treatment (prostaglandins eye drops). After the measurement of IOP by Goldmann tonometry and of blood pressures by Riva-Rocci sphygmomanometry, the mOPP was calculated according to the formula mOPP = [2/3 (2/3 dBP
+ 1/3sBP) - IOP], at three time points (8am, 2pm, 8pm). The data were shown as mean ±standard error of the mean (SEM). The statistical analyses were carried out using SPSS 24.0. The IOP and the mOPP measurements were compared in every studied group by means of ANOVA for repeated measures. A p value <0.05 was set as significant.
Results:
Sex ratio and mean age were as follows:
NTG: male (M): female (F)=10:12, mean age 70.0 ±0.6 years; HTG: M: F=10:11, mean age 70.3 ±0.6 years; and XFG: M: F=11:11, mean age 71.3 ±0.9 years.
The IOP and mOPP values significantly varied throughout the day in all the three study groups (p<0.001 for all the comparisons) (figure1). Both variables showed significantly larger fluctuations in the XFG eyes than in the NTG and HTG ones (p,0.001 for IOP and p=0.001 for mOPP) (figure 2).
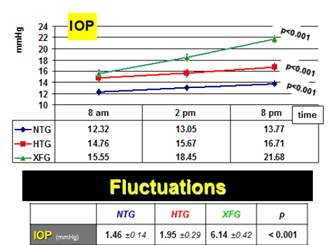
Figure 1. Diurnal IOP course
in the three studied groups
(graph, above). Comparison of IOP diurnal fluctuations among
the three studied
group
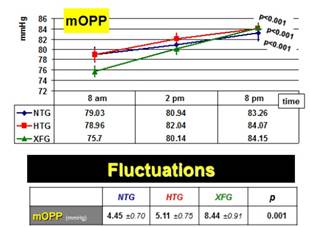
Figure 2. Diurnal mOPP course in the three studied groups (graph, above).
Comparison of mOPP diurnal fluctuations
among the three
studied group (table, below).
Discussion:
Hypertensive glaucoma (HTG), normotensive glaucoma (NTG) and exfoliative glaucoma (XFG) are the most common types of glaucoma [2-5]. They have in common typical optic nerve and visual field alterations, and differ for the weight that various risk factors have in the onset and progression of the disease.
Among the risk factors for glaucoma, high intraocular pressure (IOP) is the most important one, but reduced optic nerve blood supply has a relevant role too.
Elevated IOP is the most evident risk factor for HTG and XFG, but low mOPP has been described as well [6-10]. On the contrary, in NTG IOP is normal by definition, and low mOPP has been considered the main risk factor [11-15].
IOP can be precisely measured by tonometry, while a parameter called mean ocular perfusion pressure (mOPP) is a good estimate of the optic nerve blood supply. This parameter takes into account systemic and diastolic blood pressure (sBP and dBP) measurements and is calculated using the formula: mOPP = [2/3 dBP + 1/3 sBP] – IOP [16].
Both IOP and mOPP physiologically vary throughout the 24 hours. However, these fluctuations have been reported to be larger in glaucoma subjects than in healthy controls [17,18].
The few published papers have by far suggested that diurnal variations of IOP and mOPP may influence the severity and the progression of glaucoma [19-25].
To date, no clear data about differences in such variations among different types of glaucoma are available. We designed and conducted the following study to contribute to the research on this subject. The assessment of our findings can be more objective on a larger series.